This 3-part series dissects all aspects of a hysterectomy, inclusively covering the needs and questions of transpeople of all identities who are interested in this procedure.
Brief Un-Medical Summary
Since I don’t undertake anything without substantial research beforehand, I learned a lot about the “female” reproductive system and its removal thereof in the weeks preceding my own hysterectomy. Moreover, I had no clue what the surgery itself entailed, as well as what pre-op and post-op experiences were like.
If you’re equally confounded, or just curious about a hysterectomy, follow along in this 3-part series specifically aimed at transguys, men, genderqueer, non-binary, and otherwise trans people.
Here’s a condensed version of my learnings as a non-medical non-professional. Most of this points to other (infinitely more useful and detailed) articles which you should check out.
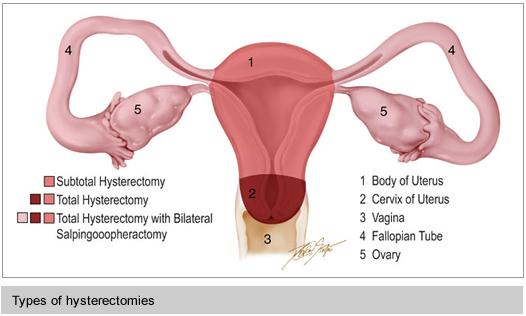
Types of Hysterectomies
Though typically thought of or referred to as removal of the uterus, a hysterectomy can be removal of any combination of parts of the “female” reproductive system. These parts include uterus, cervix, vagina, fallopian tubes, and ovaries.
The type indicates which parts are kept and/or removed.
- Radical: uterus, cervix, and ovaries removed
- Total: uterus and cervix removed
- Subtotal or Partial: uterus, or portion of
Frankly I found this terminology confusing and sometimes conflicting, so I stuck with expressly stating which parts I was keeping and/or removing each time I referred to my surgery.
Removal of the cervix is recommended in most cases. If you don’t remove it, you will need pap smears and are at risk for cervical cancer, and there is a slight chance for continued menstruation (if you are not on T). The possibility of pelvic prolapse is unclear, but my research indicates it is unlikely in most cases. (Read this article for more info.)
Furthermore, a salpingectomy refers to removal of the fallopian tubes, while an oophorectomy refers to removal of the ovaries. While commonly performed together, it’s not a necessity – that is, you can get your tubes removed and leave in the ovaries. (More on this in the next article.)
Techniques for Hysterectomies
The way this surgery is performed is varied, and primarily affects your recovery as well as visible scars.

- Abdominal: an incision in the lower abdomen along the “bikini line” (wherever that is). This is an invasive surgery, as the incision cuts through skin and abdominal muscles.
- Vaginal: everything is done through down there.
- Laparascopic (robotic and non-robotic): Three or four tiny (5mm) incisions are made in your belly button and lower abdomen, through which a camera and surgical instruments are inserted, and everything is performed via fancy machines. This technique is perhaps the most common for voluntary hysterectomies and is definitely the best option, since it’s the least invasive, leaves minimal scarring, and has a significantly faster recovery time.

To be a candidate for a vaginal or laparoscopic hysterectomy there are a few factors involved, such as not having an enlarged uterus due to childbirth or fibroids, or not having too much abdominal scar tissue due to previous operations.
The Surgery
A hysterectomy is an outpatient procedure, with the patient going home typically the same day or the day after. It lasts about 3 hours, and the biggest risks for complication is nicking the bladder or other internal organs, as well as the usual ones associated with major surgery and anesthesia.
Pre-Op
The day before surgery you undergo a very special “bowel prep” diet, which came as an unpleasant surprise for me. It involves ingesting only clear liquids and potentially laxatives for 24 hours, which empties your bowels and intestines in order to make room for the surgeon to see and to avoid accidentally cutting into them. It is not the funnest thing in the world, so you just have to suck it up.
Recovery
Full recovery is 4-12 weeks, but this varies greatly depending on the the type of surgery.
Abdominal hystos need more time to heal. It takes a while to rebuild abdominal muscles, and some people can have a hard time getting up and moving around for a few days or weeks. Usually an overnight stay may be advised, and of course there is a visible scar left.
With laparoscopy you can be up and about in a few days or so. The main complaint during recovery, other than cramps, is gas build up, since CO2 is pumped into the belly, which enables the surgeon to see all your organs. This lasts only a few days.
I was back to “normal” in just under a week, meaning I was able to resume all my daily activities excluding exercise in just under 7 days.
So why 4-12 weeks recovery time for a laparoscopy if you’re back on your feet in a few days? Because there are stitched up incisions on the inside of your organs, so you have to limit yourself to “couch potato activity levels” (my surgeon’s term) to avoid rupturing them. Especially advised is no penetrative sex and no heavy lifting for the entire recovery period. So, just prepare to have your workout (and possibly bedroom) routine interrupted for a few weeks.
Up next…
In the next two articles I’ll discuss pro’s and con’s of a hysterectomy particular to trans people, as well as the specific steps for making it happen.
Resources
- Dr. Kate O’Hanlan, a gynecologist in the San Francisco Bay Area, has published several resources specifically for Transguys getting hystos. Download her Instruction Sheet to get a good idea of everything that is involved.
- Hudson’s FTM Guide
- VCH Transhealth Brochure (pdf)
- About.com: Hysterectomy Summary (not trans-specific)
- Wikipedia: Hysterectomy
Disclaimer
I’m not a medical professional. This summary is a layperson’s understanding of personal research. It may or may not be accurate.

Thanks so much for sharing! Have been thinking on and off about a hysto for awhile, so it’s nice to see some info about it.
Reblogged this on This Mongrel Land and commented:
This post is really useful and informative.
Good series! Hysterectomy gets a little less ink than other FTM surgeries it seems, and this is important information to get out there.
You can add another “hybrid” type of hysto to the list: vaginally-assisted laparoscopic. It’s a combo of, you guessed it, vaginal hysto and lap. It uses two small abdominal incisions instead of three. It’s what I had, and my surgeon claimed that it has a lower complication rate than lap, but I don’t know if that’s true or not, and I wound up with a complication. (While I had a tough time, it turned out to be a very important surgery for me, and I’m thrilled I had it done.)
I’ll keep an eye out for part 3!
Just had surgery (hysterectomy, savings-oophorectomy) last Tuesday. I feel great! Everything’s gone perfectly!
Laparoscopic presents the potential risk of spreading undetected cancer in fibroids. From what I understand, there isn’t much an option to test for confirmation/denial of cancerous cells in fibroids prior to removal.
I was told by a gynecologist that it may be difficult to conduct a laparoscopic surgery on a transmale due to the testosterone strengthening the pelvic floor. Does this sound normal? Also, do you experience hot flashes and mood swings after the radical hysterectomy? I was told we then have to up our testosterone dosage due to a complete lack of hormones.
From what I understand, being a trans man or on testosterone should not impact eligibility for laparoscopic surgery, though other factors might.
If you remove your ovaries, you usually lower your T dosage, and might want to consider supplementing it with low estrogen as well. If you keep your ovaries, nothing should change in your dosage.
I did not experience any hot flashes or mood swings or other side effects.
No, I’ve been on T ten years. On my third week of recovery. Had radical/ total historectomy, lapriscopic, delivered through bottom hole. I’m also a mechanic and auto shop owner, so I’m a stocky little brick. Everything got removed fine, they found, endomitriosis, ovarian cyst, filopian cyst. Got it covered cause had a c-1 cervical cancer. I always denied getting a pap check for obvious reasons. For my summer physical for t refill, I got talked into one. No regrets, caught so eirly, didn’t need chemo or other treatments. It comes down to a skilled knowledgeable surgon. The lapriscopic technology is outstanding. Now they have a new tool that leaves a puncture, and one 3cm scar. The internal vag stitch is the worst, long time to heal. Feel like there is a wire pulling the gut. Best advice is to follow all prep and post op advice. Keifer milk is the best for pain killer constipation, trust me, first week on the pot may cause tears.
Good to know! Do you experience mood swings or hot flashes? I was told it might be difficult to regulate my hormones after a radical hysto and that it could effect my moods. That makes me nervous because I’m already suffering with general anxiety disorder and I’m a sensitive person so I don’t need more mood issues.
If you take your ovaries out, you might have a period of adjustment, even if you’re on T, and your dose will also change. Sometimes a small dose of estrogen is recommended as well.
Hot flashes, definitely, wakes me up at night. T alone will cause mood swings. I have actually calmed down a lot in the last few months. I’m not worried if miss my shot I’ll start bleeding. My medical records now say male. It takes time to get settled and used to the changes. My chest exploded with hair, like within a few weeks. It depends on genetics. I have a receding hairline and male pattern baldness, I had a friend who never lost a hair. It’s cool cause me and my brother’s are balding together. If I don’t take t my moods are worse and I have no energy. Do what’s best for you, but not having the body fight and regulate extra hormones feels good. I take extra D3 and Calcium as a precaution. Good luck!
Hi, thank you for that post. I’m a trans guy getting an hysterectomy in 4 months so it’s nice to know more about the recovery. I was wondering if you knew if I would be well enough for a 8 hours car trip 10 days after surgery(I know everyone is different, but in general). I wouldn’t be driving. Just sitting for 8 hours (with a small break in the middle of course).
And I know you can’t work out, but can you walk for a long time after a week or two? Like more than an hour?
I’m only seeing my doctor again in may so I can’t really ask him until then and I’m trying to see what I will be able to do this summer. 😛
Thank you.
I’m assuming you’re having this laparoscopically, otherwise the timeline is much longer.
I actually took a company field trip 7 days after surgery, and was perfectly fine. The first few days were very painful, but after that the recovery is really quick. I felt a little tired, like getting over a really bad flu. On day 14 I hopped on a plane to visit home, about a five hour flight plus everything in between.
Your body is healing on the inside, but on the outside you feel fine, so it’s mostly reminding yourself to take things easy, no carrying things and no heavy exertion.
Thank you for your anwser! I was also planning on maybe taking a plane to go somewhere, but I thought I wouldnt be able to. Now I’m going to reconsider that option. Thanks again.